U.S. Secretary of Health & Human Services (HHS) Xavier Becerra today ordered an extension of the public health emergency, citing a result of “continued consequences” of the COVID-19 pandemic. The emergency declaration had been set to expire Jan. 16.
Thus far, the public health emergency has been thus extended approximately every three months or 90 days since its initial declaration by former HHS Secretary Alex Azar II on January 27, 2020. Azar last determined a renewal in October.
An HHS spokesperson told Hospice News that the agency will “provide states with 60 days’ notice prior to any possible termination or expiration in the future.”
Hospice providers and stakeholders had urged HHS to extend the declaration, which provides essential support and flexibilities to hospices and palliative care providers in the face of record-breaking COVID surges, according to the National Hospice and Palliative Care Organization (NHPCO).
“The declaration has provided the hospice and palliative care community with necessary resources and flexibilities through approved Section 1135 waivers, allowing critical services to be provided via telehealth, and flexibility for some Medicare Hospice Conditions of Participation,” said NHPCO President and CEO Edo Banach in a recent letter to HHS Secretary Becerra. “The waivers have enabled hospice and palliative care providers to respond effectively to the urgent and complex needs of patients and their families and to limit the exposure to COVID-19 by patients, families, and staff. Until the pandemic begins to subside, assistance and flexibility from the federal government is crucial.”
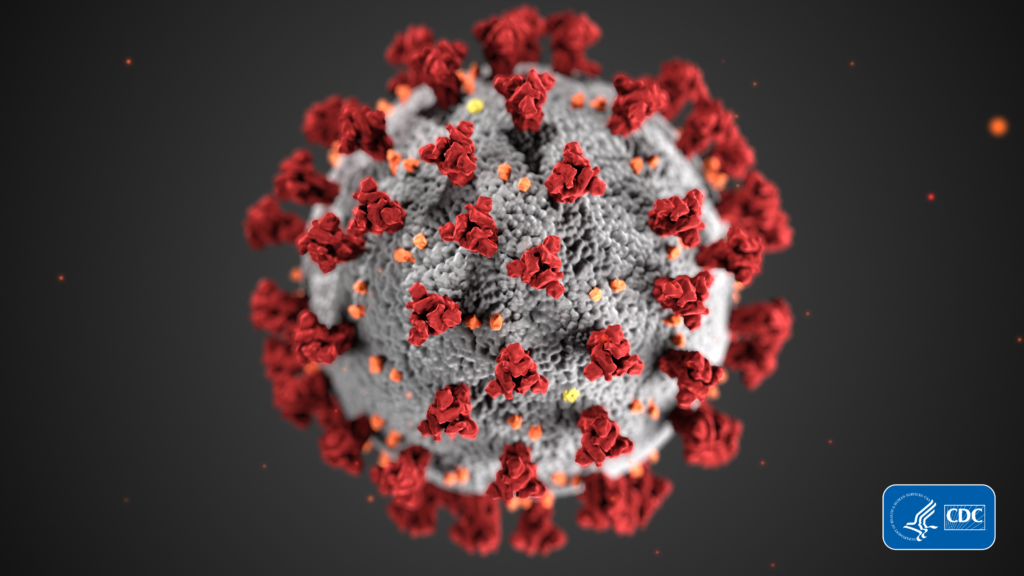
The deadly virus has claimed nearly 843,000 lives nationwide since first hitting the United States almost three years ago, according to recent data from the U.S Centers for Disease Control and Prevention (CDC).
The spread of COVID-19 has spiked in recent months, with the omicron variant gaining prevalence. On Tuesday of this week alone, a record of more than 1.4 million new cases were reported nationwide, according to John Hopkins University.
COVID-19 has pummeled hospice operations and finances and worsened long-standing staffing shortages in the industry. Providers have seen costs rise for supplies, traveling nurse services and paid sick leave as employees fall ill or become exposed to the virus, among other financial pressures. This has occurred while many providers have seen patient census and length of stay decline due to COVID-19 diagnoses and prior care delayed due to pandemic-related concerns.
A continued federally declared emergency allows flexibilities instituted by the U.S. Centers for Medicare & Medicaid Services (CMS) to remain intact, such as 1135 waivers of certain hospice rule. These flexibilities permitted the use of telehealth to fulfill requirements typically done in-person, such as recertifications by physicians.
Other exemptions have included the temporary removal of the requirement that a registered nurse or other skilled professional make an annual, onsite supervisory visit for each aide, as well as an annual assessment of the skills and competence of all individuals furnishing hospice care, and in-service training and education programs.
Companies featured in this article:
John Hopkins University, National Hospice and Palliative Care Organization