Health care workers and long-term care residents are among the highest priority groups as a coronavirus vaccine rolls out across the United States. While enthusiastic about the opportunity to protect staff from COVID-19, hospices remain concerned about vaccination storage costs and increased labor and operational expenses.
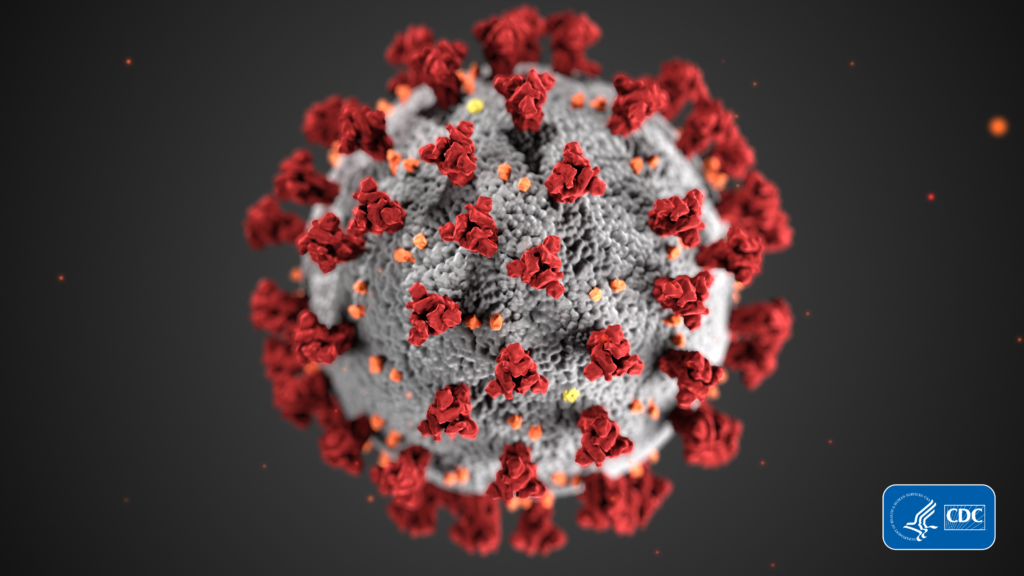
The U.S. Food and Drug Administration (FDA) issued the first emergency use authorization (EUA) for the Pfizer-BioNTech COVID-19 vaccine on Dec. 11 to prevent the coronavirus disease. Initial supply of the first 6.4 million doses will be limited and distributed across the country in phases.
Earlier in the month, the U.S. Centers for Disease Control & Prevention (CDC)’s Advisory Committee on Immunization Practices (ACIP) released an interim recommendation for highest priority levels as states determine first allocations. Health care workers and long-term residents represent roughly 17.6 million people who received the first COVID-19 vaccine. Home care and hospice staff are included in the first group (Phase 1a) because the workforce falls within ACIP’s definition of health care workers.
“Being at the front of the line for vaccinations is essential to limiting spread of COVID-19 while protecting the frontline health care workforce as well as the patients and families that hospices serve in their community,” said Hannah Yang Moore, chief advocacy officer at the National Hospice & Palliative Care Organization (NHPCO). “The overarching financial concern among hospices is the labor costs associated with staff time dedicated to getting vaccinated. Where these vaccines will be accessed will greatly impact the costs to the hospices.”
The cost of the first round of COVID-19 vaccines will initially be covered by the government, with doses federally purchased by U.S. taxpayer dollars, according to reports from the CDC. Long lines are building at state health departments allocating the vaccinations as health care workers turn out in droves, causing strain on an already depleted hospice and palliative care workforce.
Despite federal funding for the first vaccine shipments, hospice providers anticipate increased costs around the delivery and storage of vaccinations. Staff who receive the vaccination may need additional time off to cope with side effects, adding to increased paid-time off expenses hitting hospices’ bottom lines during the pandemic.
COVID-19 vaccines need to be refrigerated and administered in two rounds of doses with a waiting period in between. Operational costs add up as hospice back office staff coordinate and document employees who receive the vaccination.
“The financial impact on agencies is yet to be determined,” said Sharon Branham, president and CEO of Appalachian Hospice Care, Inc. “Cost is associated with administration of the vaccine [and] staff will need to be monitored after receiving the vaccine. To be safe, staff will need to be monitored after the dose is given. A consideration of acquisition, time and scheduling changes impact hospices financially.”
Some factors could potentially mitigate any financial damage. Vaccination costs may qualify as valid COVID-19 related expenses falling under the CARES Act, with hospices among the providers awaiting further federal guidance. Vaccine-related expenses associated with staffing issues could be offset by federal aid from the Provider Relief Fund intended to mitigate hits to providers pummeled by the pandemic, according to Yang Moore.
Fundraising and philanthropic efforts could help offset costs as hospices work to keep their staff healthy. Competition may drive down future costs as more vaccines become available. Massachusetts-based Monderna Inc. (NASDAQ: MRNA) is anticipated to be among the next in line to bring a COVID-19 vaccine to market.
Despite the costs, a strong business case exists for vaccination. It could allow hospice clinicians to regain access to patients in nursing homes and other facilities, which has been limited severely due to infection risk for vulnerable residents.
“We believe that the importance of getting our staff vaccinated will outweigh any direct expenses which may involve only the time spent by our staff in getting the vaccine,” David Donenberg, chief financial officer of Seasons Hospice and Palliative Care, told Hospice News. “Having the vaccine will allow our staff the much-needed freedom to gain access to skilled nursing facilities and hospitals to serve our patients with confidence and compassion.”
NHPCO released a statement encouraging hospice providers to get vaccinated as soon as they can gain access. Vaccination would reduce the likelihood of infection, reduce the severity of symptoms in the event of infection and protect people with whom hospice staff interact.
“For their own protection, the safety of those under their care and the welfare of their families and communities, NHPCO encourages these dedicated professionals to receive the COVID-19 vaccine,” said NHPCO President and CEO Edo Banach.
Companies featured in this article:
Appalachian Hospice Care, BioNTech SE, Moderna, National Hospice & Palliative Care Organization, National Hospice and Palliative Care Organization, Pfizer, Seasons Hospice & Palliative Care