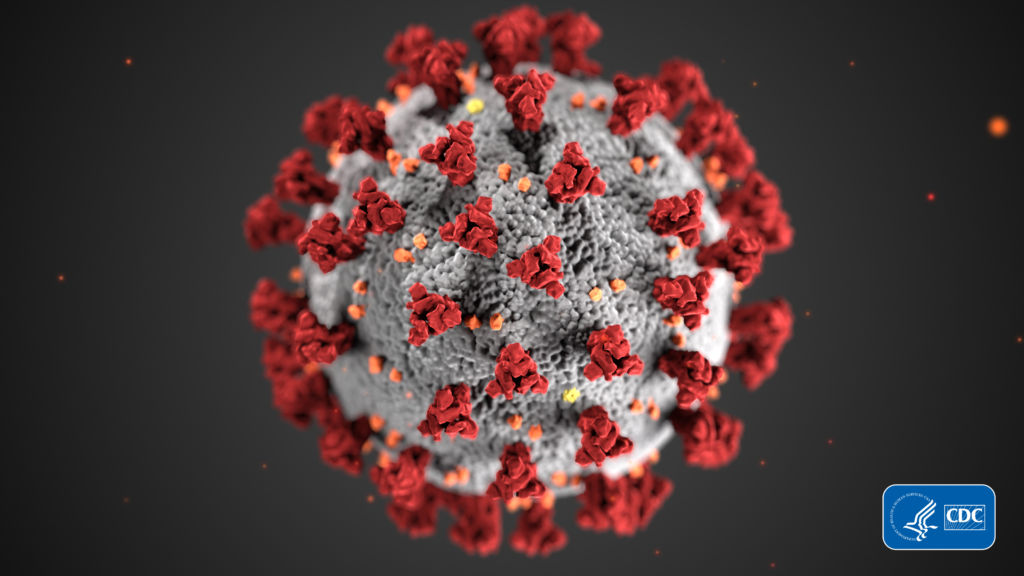
The rapid spread of coronavirus jolted the nation’s health care systems, illuminating breakdowns and deficiencies in the delivery of acute, serious illness and end-of-life care. With millions of Americans falling ill to the virus and thousands dying, a heightened focus has fallen on hospice and palliative care as providers seek to learn from the COVID-19 experience and grasp the long-term impacts.
According to the U.S. Centers for Disease Control and Prevention (CDC), there have been nearly 8 million COVID-19 cases and more than 200,000 deaths reported in the United States since the first of this year. Hospices contended with several issues as the pandemic progressed such as limited access to patients in facility-based settings, medication shortages, staff shortages and limited availability of personal protective equipment (PPE) to help protect vulnerable patients. With these issues and more among facing financial headwinds, hospice providers have much to learn from the public health crisis.
“Amidst the crises that we’re all living through, we now have new clarity about where we’ve been and where we are now that can inform where we’re going,” said Ira Byock, M.D., founder and chief medical officer of the Institute for Human Caring during a speech at the National Hospice & Palliative Care Organization (NHPCO) Interdisciplinary Care conference. “I have kind of gotten a sense of two alternate futures: one bright one in which we are living examples of the values and vision of the founders of this field; and the other not so bright in which we progressively shrivel into a husk of that vision, becoming a transactional, commodified version of what founders of hospice and palliative care had hoped to build. I believe that we are in yet another inflection point in that journey.”
The Institute for Human Caring is a component of Providence St. Joseph Health headquartered in Washington. According to Byock, hospice and palliative care providers should heed concern when realigning marketing efforts.
Misconceptions about the nature of end-of-life and serious illness care have continued to proliferate, with public perception limiting expansion of hospice and palliative care. Many providers have joined a nationwide trend in updating their public image to reflect more diversified service offerings and reach patients further upstream in the health system to dispel common myths and misunderstandings around terminal and chronic care. Several have begun rebranding to reach wider markets, hitting familiar roadblocks in communicating the value of hospice.
“We in these fields need to ask ourselves if we are really communicating effectively, and does that communication enhance the likelihood of people asking for or accepting the services that we want to offer,” said Byock. “Avoiding the words ‘death,’ ‘dying,’ ‘suffering’ and ‘hospice care’ return us to acting out of fear of being misunderstood, fear of being rejected by patients, fear of not being able to serve patients who need and would benefit from our services. Those are all legitimate concerns that we really need to address in creative ways. I suggest that in our branding we are about well-being through the end of life and we are not simply the death and dying movement. We are a part of the wellness movement, we are about well being through the very end of life, we provide the best care possible for living as fully as possible among the people who matter most to us through the end of this life. Our ‘brand’ is then that we provide the best care possible to help people live fully and die well.”
Along with heightened awareness of public perceptions, the pandemic has drawn a greater focus on the accessibility and delivery of hospice care as more patients receive services in the home setting. Many in the home health and hospice space have observed that fears of COVID-19 and dwindling bed capacity is leading to more patients receiving care in the home setting rather than an institution.
“If anyone had any doubt about whether or not hospice and palliative care is essential, I think that doubt has been wiped out through all of this pandemic,” said Edo Banach, president and CEO of NHPCO. “It’s not an option to focus on interdisciplinary care, community-based care and equity. Even with the ongoing focus on COVID-19, quality of care has to be a fundamental issue that we can’t ignore. It’s been incredibly clear to me, and I think to a lot of people that have been paying attention, that the person- and family-centered care that we provide is necessary. It’s important and it’s essential. We need more of it within our health care landscape. The value of the interdisciplinary care team, which is the hallmark of hospice and will be the hallmark of community based palliative care, is becoming acknowledged and I think that is here to stay.”
Telehealth has become a common avenue hospices have employed to continue reaching patients and their families in the home and various settings under loosened restrictions during the pandemic. As the U.S. Centers for Medicare & Medicaid Services (CMS) plans to make permanent some of the temporary flexibilities expanding telehealth utilization in response to the pandemic, it remains to be seen which rules will impact the hospice space. Hospice providers have built up telehealth utilization for both medical visits and non-medical services. With patient and family support increasingly available with virtual and online avenues, providers stand to benefit from an expanded digital reach.
Hospice providers will face continued challenges in striking a balance between virtual and in-person care as they look ahead and incorporate technology further into services and programming.
“Telehealth is something that we’ve been talking about for such a long time. It’s here now, and it’s here to stay,” said Banach. “It’s our job to make sure that those things that we can do virtually, we’re able to do safely and those things that that we can’t, we still provide in person. We have to get the balance right. If it’s true that we’ve got a grieving nation, if we’ve got depression and social isolation, then telehealth is not going to get us out of that. So while we’re excited about telehealth, we have to make sure that we use it as a supplement to in person care and not as a replacement.”
Companies featured in this article:
Institute for Human Caring, National Hospice and Palliative Care Organization, Providence St. Joseph Health