Infection control is at the heart of hospice and palliative care providers’ response to the COVID-19 crisis as these organizations care for some of the most vulnerable patient populations. While infection control is certainly not a new topic in health care settings, new questions are arising during the pandemic about best prevention practices to protect patients, families and hospice staff.
Hospices are working to ensure that staff not only have access to personal protective equipment (PPE) amid widespread supply shortages, but also that they know how to use it effectively. Most hospice care and a growing proportion of palliative care is delivered in patients’ homes, which adds the ongoing challenge of assessing each patient’s home environment, including for infection risk points.
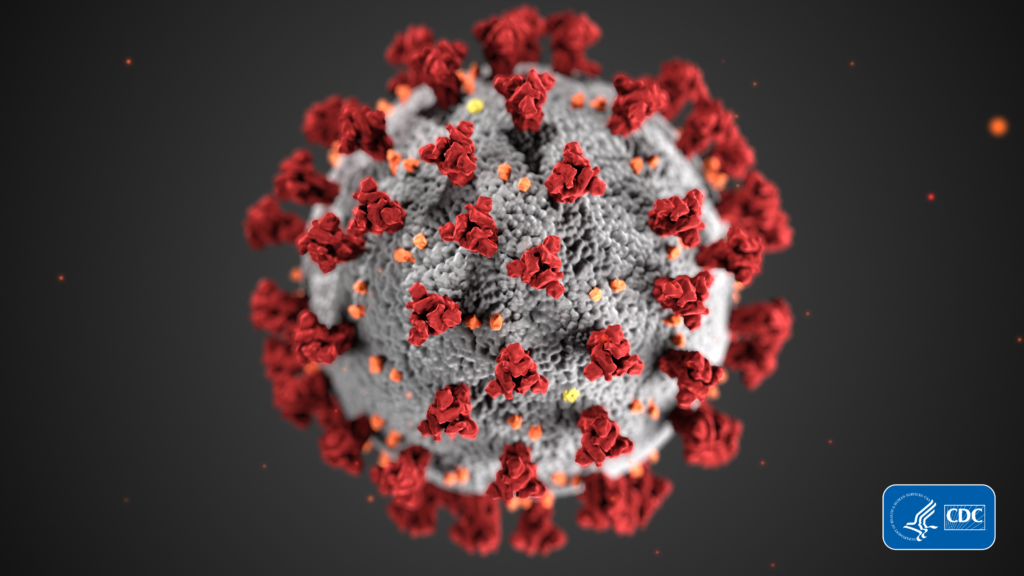
Working in hospices’ favor is the reality that field staff are accustomed to following infection prevention guidelines set by health agencies, such as the U.S. Centers for Disease Control and Prevention (CDC), the World Health Organization, and other entities, to help ensure their own safety and that of their patients.
“You’re still going to be using the same prevention practices,” said Missy Ring, director of regulatory and quality for the National Hospice & Palliative Care Organization (NHPCO) in a recent podcast. “Adding on with this layer in your infection control of potentially having a COVID-19 positive patient or someone exhibiting symptoms. What people are going to have to tap back into is all of the training, what they learned when they were taught in their orientations of what to do when you’re entering these [patient] homes.”
Hospices are faced with questions about how to apply infection prevention and control protocols given the unique aspects of the pandemic; for instance, the question of whether to rely more on handwashing versus alcohol-based hand rubs, which is often in short supply. In an effort not only to stretch supplies but also effectively protect themselves and patients, hospice and palliative care staff are learning to balance their needs against their available resources.
“Whatever you have that’s quickly available in that environment,” Ring suggested, stressing that the patient’s well-being and safety are of greatest concern, right along with the clinicians’.
As the pandemic evolves, several risk factors will continue to come into play as hospice providers reevaluate infection prevention mechanisms in both the home and facility settings. Hospice staff have had to take more stringent measures during the pandemic than during normal operations.
“Now we cannot afford to be less vigilant in following these guidelines because of how quickly and how varialant this virus is and the transmission and spread of it,” said NHPCO Senior Director of Regulatory and Quality Jennifer Kennedy in the podcast. “So, making sure that you’re using your [clinical] skills is more important than it’s ever been before. And those simple but effective government best practices and guidelines don’t stop, and that’s what we have to remember — to continue those practices.”