As the health care system strives to care for the legions of patients suffering from COVID-19, hospices have accepted an influx of patients who are infected with the virus. With hospice and palliative care patients among the most vulnerable to coronavirus disease infection, providers have ramped up infection control efforts to protect those at highest risk. In the midst of this, hospices have had to get creative as to how they help infectious patients safely maintain contact with their families.
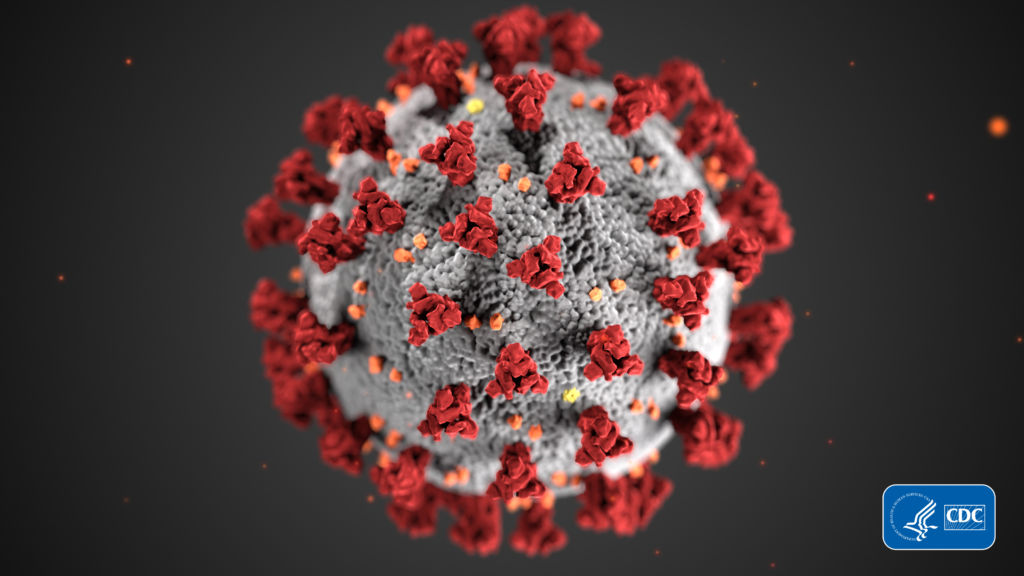
The virus has significantly impacted end-of-life care as hospices respond to the challenging needs of COVID-19 patients and their families. Nearly 11,000 COVID-19 patients died in their homes thus car in the pandemic, according to a report last week from the U.S. Centers for Disease Control and Prevention (CDC). The proportion of those patients who were receiving hospice care is currently unknown, but more than 6,000 COVID-related deaths nationwide have occurred in a hospice facility.
“Hospice and palliative patients are high risk not just for COVID-19, but susceptible to any virus, cold or flu. They are individuals with a chronic illness that entails a vast number of comorbidities,” said Shelley Cartwright, CEO of Illinois-based Apex Hospice and Palliative Care. “Their immune systems are challenged and moments of exposure and possible contraction of COVID-19 are life threatening. The rallying of family improves the quality and end-of-life experience, it brings peace to the patients. The unique need of these patients and their families is the emotional connection between the two, which has changed because of the pandemic. This was taken from patients and families as the pandemic evolved.”
Apex has seen 47 COVID-19-positive patients, with 80% exposed or testing positive stemming from skilled nursing facility referrals or contracting the virus from family members at home, according to Cartwright. Of these patients, many died within 24 hours of being admitted.
No hospice is immune to COVID-19. Small and large organizations alike have contended with upticks of COVID-positive patients as the pandemic’s continued spread creates various “hotspot” pockets along its path. Louisiana, New York and Washington were among the hardest hit early on in 2020, with Midwestern and Southern regions such as Illinois, Wisconsin and Florida joining the fight in summer months.
Headquartered in Louisiana, LHC Group (NASDAQ: LHCG is among the nation’s larger home health and hospice care providers. The company has seen thousands of COVID patients across its service lines.
“We’ve seen a number of COVID patients, over 9,000, in our home health service line year to date that were coming in as positive or suspected,” said Joshua Proffitt, president of LHC Group, during an episode of Hospice News’ Elevate podcast. “We have cared for almost 500 COVID patients in our hospice service and we are really proud of that.”
Some providers have made significant changes to their operations in response to the coronavirus. Some have even expanded their services to meet the growing need.
In April, Heart of Hospice opened a dedicated COVID inpatient center in the New Orleans area that has since become a permanent facility available to patients with any terminal diagnosis, including the coronavirus. Daily screening, weekly testing and protective personal equipment (PPE) were some of the strategies employed to care for COVID-19-positive patients, along with providing education to family members, advance care planning consultations, and interdisciplinary televisits with physicians, social workers and spiritual care teams.
“To date, Heart of Hospice has cared for more than 460 COVID-19 positive patients. In Louisiana alone, where one of the nation’s major hotspots erupted, we have cared for 387 patients,” said CEO of Heart of Hospice, Carla Davis. “We are honored to have served approximately 7% of all individuals who died from COVID-19 in the state. COVID-19 impacts all individuals differently, but the majority of patients we admitted to our services were made eligible by the presence of one or more comorbid conditions. As soon as the pandemic began impacting our communities in the Southeast, we knew we would serve COVID-19 positive patients who needed our help.”
Heart of Hospice was not the only provider that implemented new services to care for COVID-19-positive patients, many of whom face challenges of isolation and reduced caregiving and family support with the need to socially distance to minimize exposure risks.
“We were very concerned about our beds being limited — and we got close capacity-wise — so we opened up a separate unit to accept patients coming from the hospital who were clearly dying,” said Christopher Kerr, CEO and chief medical officer of Hospice & Palliative Care Buffalo in New York. “We lost 80 patient lives to COVID, and that’s also 80 very disconnected family members. If there was ever a call for holistic, unifying care, it’s during a pandemic where people are isolated and disconnected. One of the roles we’ve tried to play for family members who were not able to see their loved one at a hospital or nursing facility was to actually transfer them into our care so that we could better connect a dying patient to their loved one. That liaison role as a bridge to connect them became very, very important and really honors the intent of the hospice benefit, which is that we treat people in totality — including their family.”
Hospices have increasingly leveraged technology to keep COVID patients virtually connected with their families, utilizing temporary telehealth flexibilities implemented in response to the pandemic by the U.S. Centers for Medicare & Medicaid Services (CMS). Striking a balance between human touch and technology has become a struggle during the pandemic. Disenfranchised grief has been an additional concern as providers move bereavement support services online.
“COVID-19 has caused a change that goes against the grain of the hospice philosophy,” said Cartwright. “A significant component of hospice is to unite patients with their family members, providing support of emotional, social and spiritual needs. Symptom management and comfort is always the goal, but only one element of what hospice provides. The rallying of family improves the quality and end-of-life experience. It brings peace to the patients.”
Companies featured in this article:
Apex Hospice and Palliative Care, Heart of Hospice, Hospice and Palliative Care Buffalo, LHC Group