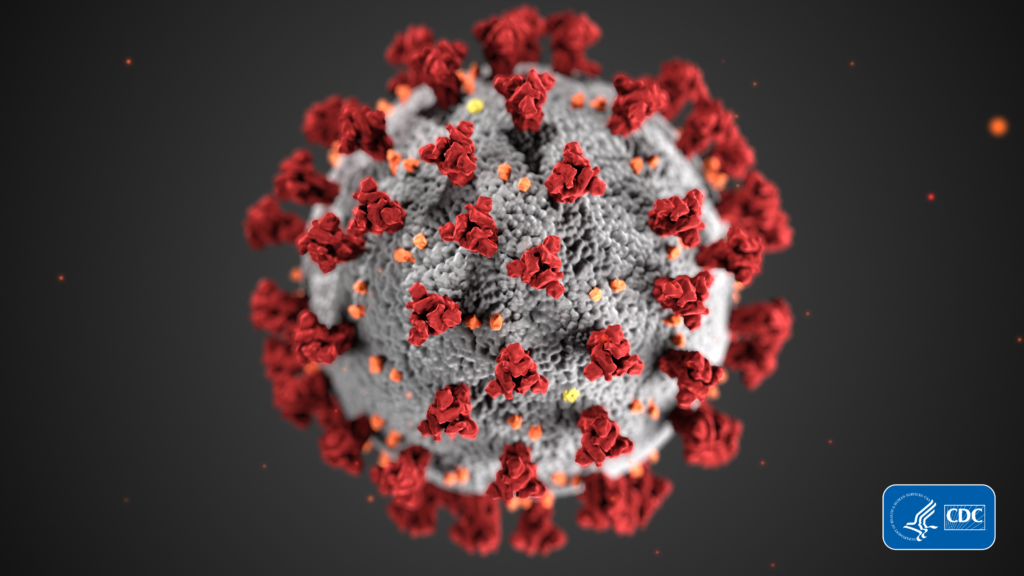
The health care community is bracing itself for a potential widespread outbreak of the COVID 19 coronavirus strain, and hospices are no exception. While hospice patients are in their final days, preventing infections that could cause greater suffering remains essential to the hospice mission.
Patients infected with COVID 19 have presented in nearly 70 locations worldwide, according to the U.S Centers for Disease Control and Prevention (CDC). In the United States about 100 cases have been identified in 13 states thus far, resulting in 11 deaths. California and Washington are hardest hit with more than 30 cases reported in each of those states.
Though none of the reported cases involved hospice patients, providers are taking steps in case their patients, staff or operations are impacted. The White House and the CDC are expected to release prevention and response guidelines for health care organizations who provide care in the home and community in the near future. On March 4, the government issued guidance applicable to hospitals and nursing homes.
While hospices are taking the prospect of a mass outbreak seriously, leaders in the space also note that such an outbreak has not yet occurred and caution against overreaction.
“As hospice and palliative care providers we have a unique ability to disseminate information and to provide care in some pretty uncontrolled circumstances,” Edo Banach, president and CEO of the National Hospice & Palliative Care Organization (NHPCO), told Hospice News. “[Providers] are addressing the threat through education, letting their communities and staff know about some best practices. I want to stress that where we are right now influenza is much more common and more deadly.”
Banach and other representatives of the hospice community attended a March 5 meeting at the White House with Vice President Mike Pence to discuss the implications of COVID 19. Pence is heading up the federal response to the virus.
Hospice providers have begun developing policies and procedures for responding to an outbreak and educating employees about what to do if they suspect they have been exposed or are experiencing symptoms.
The first measure most are taking is to bolster existing infection prevention and control measures, including compliance with CDC guidelines, U.S. Centers for Medicare & Medicaid Services (CMS) regulation and accreditation agency standards. These include improving hand hygiene compliance and the use of standard precautions.
Communication regarding potential exposures is also a key component, according to written policies and procedures developed by hospice and home health provider LHC Group (NASDAQ: LHCG).
“Employees must immediately report any concerns regarding exposure to 2019-nCoV to a supervisor, whether the potential exposure has occurred through providing patient care, travel, assisting an ill traveler or other person, handling a contaminated object, or cleaning a contaminated environment,” the document indicated. “Upon receipt of a report of potential exposure from an employee, the supervisor must take the following immediate actions: Ascertain and fully document: The circumstances surrounding the potential exposure as reported by the employee; whether the employee is experiencing any symptoms associated with 2019-nCoVas.”
Some providers have begun screening patients and families, particularly to determine if they have had close contact with an infected person or whether they had travelled recently to countries or regions where spread of the illness has been more rampant, such as China.
“We’ve taken proactive steps to eliminate unnecessary travel and taking steps to enhance screening practices across the organization. This is in addition to emphasizing the fundamentals of good infection control practices,” said Danny Walker, CEO of the Pennant Group (NASDAQ: PNTG), in an earnings conference call. “As we continue to monitor the ongoing situation, we will make adjustments as needed to provide the best possible support for our clinical and operational teams as they continue to provide essential care care in the communities they serve.”
In addition to safety risks, an outbreak could have serious consequences for hospices from a business and operational perspective. Employees who acquire the virus would not be able to make home visits, with many organizations already understaffed. Sick personnel could also impact back office operations.
Employees who become exposed on the job may also be entitled to worker compensation, according to the LHC Group document. The National Association for Home Care & Hospice (NAHC) provided Hospice News with the document.
Hospices are already encountering some challenges stemming from COVID 19, including supply disruption for infection control products.
“There are a couple things that we need to be able to do and we talked about a couple of them [with Pence at the White House],” Banach said. “One is the supply issue, to make sure that as we provide care we’re protecting our workforce and that we’re protecting the folks that we are visiting. These are gowns and masks and face shields and gloves.”
Should the crisis grow and infections proliferate, additional measures may be needed both at the provider and national level. It may become necessary for CMS to allow hospices a public health emergency waiver that would temporarily relax some Medicare and Medicaid requirements in heavily affected areas, according to Banach. He also said that more flexibility in regards to the use of telehealth, as well as reimbursement for those services, may be warranted to reduce physical contact that could spread illness.
The immediate risk of infection is still low for most of the U.S. population, according to the CDC. The risk is somewhat elevated in areas in which ongoing community spread has occurred and among individuals who have travelled to China or other countries where outbreaks are more rampant.
On a heartening note, hospice providers do have experience working through public health crises that generated considerable public anxiety.
“Hospice was faced with a public health challenge right after it was established [in the late 1970s and early 1980s] — HIV and AIDS. This was another time when there was an unknown disease, the spread of which was obviously feared,” Banach told Hospice News. “Precautions had to be taken to provide care to individuals, and instead of ringing our collective hands, hospice and palliative care providers stepped up and provided support to individuals when they needed it.”
Companies featured in this article:
LHC Group, National Association for Home Care and Hospice, National Hospice and Palliative Care Organization, Pennant Group